What is diabetic retinopathy?
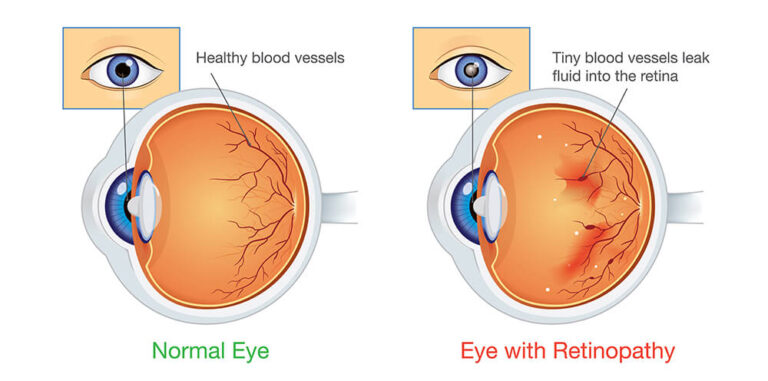
Diabetic retinopathy is an eye condition that can cause vision loss and blindness in people who have diabetes. It affects blood vessels in the retina (the light-sensitive layer of tissue in the back of your eye).
If you have diabetes, it’s important for you to get a comprehensive dilated eye exam at least once a year. Diabetic retinopathy may not have any symptoms at first — but finding it early can help you take steps to protect your vision.
Managing your diabetes — by staying physically active, eating healthy, and taking your medicine — can also help you prevent or delay vision loss.
What are the symptoms of diabetic retinopathy?
Diabetic retinopathy can lead to other serious eye conditions:
- Diabetic macular edema (DME) – Over time, about half of people with diabetic retinopathy will develop DME. DME happens when blood vessels in the retina leak fluid, causing swelling in the macula (a part of the retina). If you have DME, your vision will become blurry because of the extra fluid in your macula.
- Neovascular glaucoma – Diabetic retinopathy can cause abnormal blood vessels to grow out of the retina and block fluid from draining out of the eye. This causes a type of glaucoma.
- Retinal detachment – Diabetic retinopathy can cause scars to form in the back of your eye. When the scars pull your retina away from the back of your eye, it’s called tractional retinal detachment.
Am I at risk for diabetic retinopathy?
Anyone with any kind of diabetes can get diabetic retinopathy — including people with type 1, type 2, and gestational diabetes (diabetes that can develop during pregnancy).
Your risk increases the longer you have diabetes. More than 2 in 5 Americans with diabetes have some stage of diabetic retinopathy. The good news is that you can lower your risk of developing diabetic retinopathy by controlling your diabetes.
Women with diabetes who become pregnant — or women who develop gestational diabetes — are at high risk for getting diabetic retinopathy. If you have diabetes and are pregnant, have a comprehensive dilated eye exam as soon as possible. Ask your doctor if you’ll need additional eye exams during your pregnancy.
What causes diabetic retinopathy?
Diabetic retinopathy is caused by high blood sugar due to diabetes. Over time, having too much sugar in your blood can damage your retina — the part of your eye that detects light and sends signals to your brain through a nerve in the back of your eye (optic nerve).
Diabetes damages blood vessels all over the body. The damage to your eyes starts when sugar blocks the tiny blood vessels that go to your retina, causing them to leak fluid or bleed. To make up for these blocked blood vessels, your eyes then grow new blood vessels that don’t work well. These new blood vessels can leak or bleed easily.
How will my eye doctor check for diabetic retinopathy?
Eye doctors can check for diabetic retinopathy as part of a dilated eye exam. The exam is simple and painless — your doctor will give you some eye drops to dilate (widen) your pupil and then check your eyes for diabetic retinopathy and other eye problems.
If you have diabetes, it’s very important to get regular eye exams. If you do develop diabetic retinopathy, early treatment can stop the damage and prevent blindness.
If your eye doctor thinks you may have severe diabetic retinopathy or DME, they may do a test called a fluorescein angiogram. This test lets the doctor see pictures of the blood vessels in your retina.
What can I do to prevent diabetic retinopathy?
Managing your diabetes is the best way to lower your risk of diabetic retinopathy. That means keeping your blood sugar levels as close to normal as possible. You can do this by getting regular physical activity, eating healthy, and carefully following your doctor’s instructions for your insulin or other diabetes medicines.
To help control your blood sugar, you’ll need a special test called an A1c test. This test shows your average blood sugar level over a 3-month period. Talk with your doctor about lowering your A1c level to help prevent or manage diabetic retinopathy.
Having high blood pressure or high cholesterol along with diabetes increases your risk for diabetic retinopathy. So controlling your blood pressure and cholesterol can also help lower your risk for vision loss.
What’s the treatment for diabetic retinopathy and DME?
In the early stages of diabetic retinopathy, your eye doctor will probably just keep track of how your eyes are doing. Some people with diabetic retinopathy may need a comprehensive dilated eye exam as often as every 2 to 4 months.
In later stages, it’s important to start treatment right away — especially if you experience changes in your vision. While it won’t undo any damage to your vision, treatment can stop your vision from getting worse. It’s also important to take steps to control your diabetes, blood pressure, and cholesterol.
Injections – Medicines called anti-VEGF drugs can slow down or reverse diabetic retinopathy. Other medicines, called corticosteroids, can also help.
Laser treatment – To reduce swelling in your retina, eye doctors can use lasers to make the blood vessels shrink and stop leaking.
Eye surgery – If your retina is bleeding a lot or you have a lot of scars in your eye, your eye doctor may recommend a type of surgery called a vitrectomy.